Part 5 in our series on Dementia. Check out Part 1, Part 2, Part 3, and Part 4 here.
To no one’s surprise, wound development is a serious issue in the nursing home. More than 1 in 10 nursing home residents have a pressure injury. Residents who depend on wheelchairs for mobility are more susceptible than ambulatory residents. Our wheelchair-dependent dementia patients are at an even higher risk for pressure injuries due to sensation issues that arise as a result of the disease process. Understanding these sensation issues will help you choose the best wheelchair system for a resident with dementia.
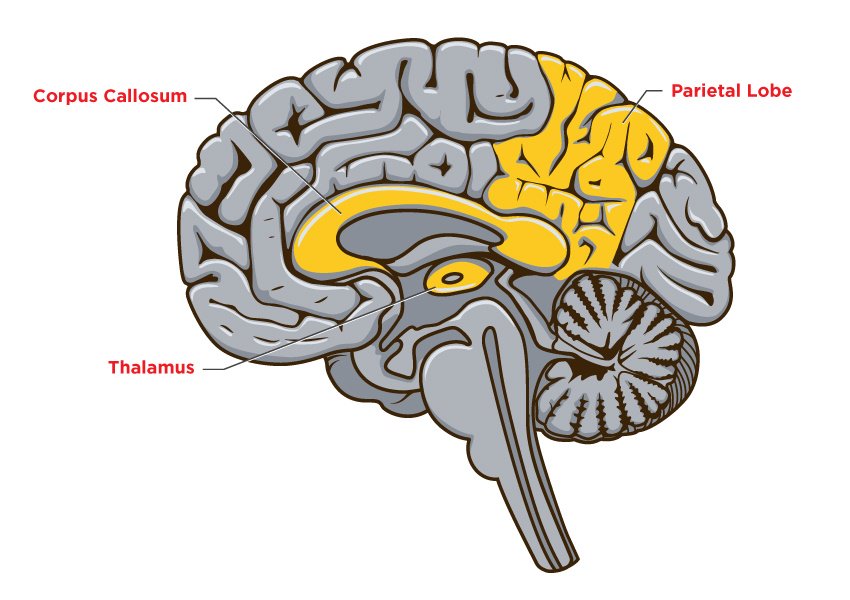
Damage to the brain at the parietal lobe, corpus callosum, and thalamus can cause an oversensitivity to stimuli and/or lengthen the processing time to noxious input and the ability to react to it in the resident with dementia. The fight or flight response is impaired. Residents will take longer to change position, ask for pain relief, or get up when compared to a resident without dementia.
Sensation issues that arise with dementia include:
- Loss of feeling
- Decreased ability to feel or regulate hot/cold
- Inability to feel the effects of pressure
- Increased processing time to recognize and express pain
- Heightened pain sensation such as burning, prickling, or pressure
- Sensation of pain intensified by cold or touch
- Decreased ability to sense when injury has occurred
Four items on this list should be JUMPING off the page at you.
- Decreased ability to feel or regulate hot/cold
- Inability to feel the effects of pressure
- Increased processing time to recognize and express pain
- Decreased ability to sense when injury has occurred
These losses make a resident much more susceptible to the extrinsic factors of wound development:
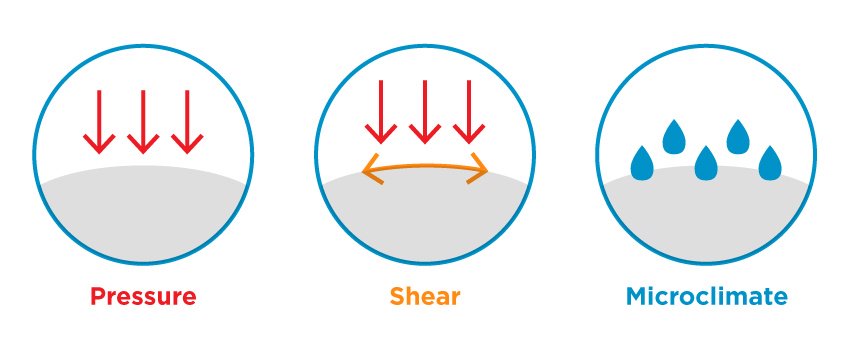
We need to safeguard the resident from the effects of pressure by utilizing proper cushions and back supports. Aim to protect the bony prominences, which, often times, are more prominent due to the loss of appetite and weight loss common to residents with dementia. Damage to the parietal lobe makes a resident unable to feel the effects of pressure at the ITs, sacrum, coccyx, spinous process, and bony landmarks of the trunk. The damage can decrease the ability to respond in a timely manner to painful stimuli.
It is not that the resident does not feel pain; the problem is that it takes them longer to process pain and seek out relief from pressure-causing pain. Studies show that it takes only fifteen minutes for damage to take place at the skin surface. However, for a resident with dementia, it may take much longer than fifteen minutes to recognize the pain and express the warning signs of a pressure wound to a caregiver.
We need to defend against shear that occurs during transfers, reaching, weight shifts, or repositioning. This is extremely important for the fidgeting resident that is agitated and continuously moving in the chair. This constant movement creates downward pressure and friction, which is known as shear. The damage related to shear is very dangerous because it starts at the deeper layers of the skin and works its way up to the skin surface. A resident with compromised sensation will be unaware of the injury until the pressure injury is at a very advanced stage.
We also need to protect the skin from a build-up of excessive heat and moisture, which is known as microclimate, as their ability to regulate temperature is now compromised. Eliminating microclimate at the seat surface is an absolute must! The effects of pressure and friction is FIVE TIMES greater when moisture is present.
WHAT CAN THE THERAPIST DO?
Let’s become the “voice” for our residents with dementia and be proactive when choosing the cushion and back support to prevent wound development. Choose cushions and back supports with skin protection properties that will defend the skin and skeleton from pressure, shear, and microclimate.
We need to look for cushions that have the correct geometry to fight pressure:
- Immerse the bony prominences to protect them from pressure.
Or
- Cushions with contour that offload the pressure from the ITs, sacrum, and coccyx to the larger femurs that can withstand the pressure. Key contours to look for are medial abductors, lateral adductors, and a deep posterior pelvic well. Contours help align the LEs and pelvis to eliminate movement that would increase pressure on unwanted areas.
Or
- A combination cushion that has both immersion and offloading properties if the resident has a severe postural deformity and skin issues.
We need to purchase cushions that offer GlideWear®:
GlideWear is a fabric applied to cushion covers under the pelvis that has a low co-efficient of friction. This allows the resident’s pelvis to move while reaching, weight shifting, repositioning, and during transfers. A cover without GlideWear has a high co-efficient of friction throughout the cushion surface and fights against the natural movement of the pelvis, causing shear.
We need to look for cushion covers that fight microclimate at the seat surface. Comfort Company fights against microclimate by offering cushions with mesh liners, incontinent liners, and GlideWear, all proven to control microclimate.
When choosing a cushion that will fight microclimate, look for descriptors such as:
- Dissipates heat
- Air and moisture permeable
- Breathable
- Moisture wicking
- Temperature regulation
- Air flow
Remember that a resident with dementia often times is unaware that his body is under attack. We need to be aware of the sensation losses a resident with dementia faces and be proactive in choosing an appropriate wheelchair system that will prevent harm and maintain the highest quality of life.
See you next week when we discuss choosing the correct wheelchair when dealing with dementia related motor issues.

Ana Endsjo, MOTR/L, CLT
Clinical Education Manager LTC Division
Ana Endsjo has worked as an occupational therapist since 2001 in a variety of treatment settings. She has mainly worked with the geriatric population, dedicated to the betterment of the treatment of the elderly in LTC centers. Her focus has been on seating and positioning and contracture management of the nursing home resident. With this experience, her hope is to guide other therapists, rehab directors, nurses, and administrators through educational guides, blogs, webinars, and live courses in her role as Clinical Education Manager for the long term care division.